The Causes, Symptoms, and Treatments of Peripheral Venous Disease
Peripheral Venous Disease: Causes, Symptoms & Treatments
Have you noticed swollen ankles after a long day or bulging veins in your legs that won’t go away? These could be warning signs your body is sending you about a common yet often overlooked condition called peripheral venous disease. Understanding this vascular disorder early can make all the difference in preventing serious complications and maintaining your quality of life.
What Is Peripheral Venous Disease
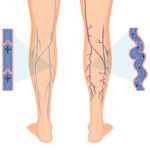
Peripheral venous disease is a circulation disorder affecting the veins in your extremities, most commonly the legs and arms. This condition occurs when veins become damaged or blocked, preventing proper blood flow back to your heart. Unlike arteries that carry oxygen rich blood away from your heart, veins work against gravity to return blood upward, relying on tiny valves to prevent backward flow.
When these valves weaken or fail, blood pools in your lower extremities, creating a cascade of uncomfortable symptoms and potential health risks. Peripheral venous disease affects millions of Americans, with varicose veins alone impacting up to 30% of adults, particularly women over age 50.
Understanding the Root Causes of Venous Disease
Several factors contribute to the development of chronic venous insufficiency and related vascular conditions. The primary mechanism involves damage to vein walls or valve dysfunction, but what triggers this damage?
Primary Risk Factors
Age plays a significant role, as vein walls naturally lose elasticity over time. People over 50 face higher risks due to decades of gravitational stress on leg veins. Genetics matters too if your parents had varicose veins or venous insufficiency, your likelihood increases substantially.
Pregnancy creates additional pressure on pelvic and leg veins due to increased blood volume and hormonal changes that relax vein walls. Women who’ve had multiple pregnancies face even greater risk. Being overweight or obese adds extra strain on your circulatory system, making it harder for blood to flow upward against gravity.
Lifestyle Contributing Factors
Occupations requiring prolonged standing or sitting can worsen venous pressure. Teachers, nurses, cashiers, and office workers often develop venous problems due to static postures that restrict blood flow. Previous deep vein thrombosis damages vein structures, leading to post thrombotic syndrome a form of chronic venous disease that develops after blood clots.
Other medical conditions like diabetes, high blood pressure, and heart disease can compromise vascular health. Smoking damages blood vessel walls and reduces circulation, accelerating venous deterioration.
Recognizing the Warning Signs and Symptoms
Early detection of venous disease symptoms can prevent progression to more serious complications. Many people dismiss initial signs as normal aging or fatigue, but recognizing these warnings helps you seek timely treatment.
Common Early Symptoms
Leg heaviness or aching worsens throughout the day, especially after prolonged standing. This dull discomfort typically improves with leg elevation or rest. Swelling in ankles and feet, known as edema, becomes more pronounced by evening. You might notice your shoes feel tighter at day’s end.
Muscle cramping, particularly at night, disrupts sleep and signals poor circulation. These cramps often affect calf muscles and can be quite painful. Restless legs, an irresistible urge to move your legs when resting, frequently accompanies venous insufficiency.
Visible Vein Changes
Spider veins appear as small red, blue, or purple web like patterns on skin surfaces. While often considered cosmetic concerns, they can indicate underlying venous problems. Varicose veins are larger, bulging, twisted veins visible beneath the skin, usually in legs and thighs. These enlarged veins may feel tender to touch and cause aching or throbbing.
Advanced Stage Symptoms
As venous disease progresses without treatment, symptoms become more severe. Skin discoloration, particularly around ankles, develops a brownish or reddish tint due to blood leaking into surrounding tissue. The skin becomes hardened and tight, a condition called lipodermatosclerosis.
Venous stasis dermatitis causes itchy, inflamed skin that may weep fluid or develop a rash. This inflammation makes skin fragile and prone to injury. Venous ulcers, open sores that typically form near ankles, represent the most serious complication. These wounds heal slowly and easily become infected, sometimes developing into cellulitis, a dangerous bacterial skin infection.
Diagnostic Approaches for Venous Disorders
Proper diagnosis begins with a comprehensive evaluation by a qualified Vascular Surgeon in Houston or your local area. Your healthcare provider will conduct a thorough physical examination, checking for visible vein abnormalities, skin changes, and swelling patterns.
Non Invasive Testing Methods
Duplex ultrasound serves as the gold standard for diagnosing venous disease. This painless test uses sound waves to create images of blood flow through your veins, identifying valve dysfunction, blockages, or blood clots. The procedure typically takes 30 to 45 minutes and provides real time visualization of circulatory problems.
Additional diagnostic tools may include venography, where contrast dye is injected to highlight vein structures on X ray images. CT scans or MRI imaging might be recommended for complex cases requiring detailed anatomical information.
Comprehensive Treatment Options Available Today
Modern medicine offers numerous effective treatments for peripheral venous disease, ranging from conservative lifestyle modifications to advanced minimally invasive procedures. Treatment selection depends on symptom severity, overall health status, and personal preferences.
Conservative Management Strategies
For mild to moderate cases, lifestyle changes form the foundation of treatment. Regular exercise, particularly walking and swimming, strengthens calf muscles that help pump blood upward. Maintaining a healthy weight reduces pressure on leg veins.
Compression therapy using graduated compression stockings provides external support that helps veins move blood more efficiently. These specialized stockings apply strongest pressure at ankles, gradually decreasing up the leg. Many patients experience significant symptom relief with consistent compression garment use.
Leg elevation above heart level for 15 to 20 minutes several times daily allows gravity to assist blood return. This simple intervention reduces swelling and discomfort effectively.
Minimally Invasive Procedures
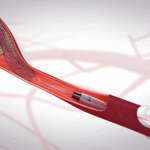
When conservative measures prove insufficient, several outpatient procedures offer excellent results with minimal downtime. Endovenous ablation uses thermal energy delivered through a thin catheter to seal problematic veins. The body naturally reroutes blood through healthier vessels.
Sclerotherapy involves injecting a solution into spider veins and small varicose veins, causing them to collapse and fade. This quick office procedure requires no anesthesia and allows immediate return to normal activities.
VenaSeal, a newer technique, uses medical adhesive to close damaged veins. This approach eliminates the need for tumescent anesthesia and multiple needle sticks, reducing discomfort and recovery time.
Advanced Surgical Solutions
Severe cases may require surgical intervention. Vein stripping removes large varicose veins through small incisions. Though more invasive than newer techniques, it remains effective for extensive venous damage.
Venous stenting opens blocked deep veins using balloon angioplasty and metal stents, restoring normal flow patterns. This procedure particularly benefits patients with post thrombotic syndrome or May Thurner syndrome.
Living Well with Venous Disease Prevention Tips
Prevention strategies can significantly reduce your risk of developing venous problems or slow progression if you already have early stage disease. Simple daily habits make a substantial difference.
Avoid prolonged sitting or standing by taking movement breaks every 30 minutes. Flex your ankles and walk around briefly to activate your calf muscle pump. Stay hydrated, as adequate fluid intake helps maintain healthy blood viscosity.
Exercise regularly, focusing on activities that engage leg muscles. Walking, cycling, and swimming all promote healthy circulation. Maintain a balanced diet rich in fiber to prevent constipation, which can increase abdominal pressure and strain leg veins.
Elevate your legs when resting, and avoid crossing your legs while sitting. Wear comfortable, well fitting shoes with good arch support rather than high heels. If you smoke, seek support to quit, as tobacco use accelerates vascular damage throughout your body.
Frequently Asked Questions About Peripheral Venous Disease
Can peripheral venous disease be cured completely?
While venous damage is generally permanent, symptoms can be effectively managed or eliminated through appropriate treatment. Modern therapies provide excellent long term results, though the condition requires ongoing attention to prevent recurrence in other veins.
How long does recovery take after venous treatment?
Recovery varies by procedure type. Minimally invasive treatments like sclerotherapy and ablation typically require only a few days of limited activity, with most patients returning to normal routines within a week. Surgical procedures may need two to four weeks for full recovery.
Are venous disease treatments covered by insurance?
Many venous treatments are covered when medically necessary, meaning symptoms significantly impact daily life or present health risks. Purely cosmetic procedures may not be covered. Check with your insurance provider and healthcare team to understand your coverage options.
Take Control of Your Vascular Health Today
Peripheral venous disease affects millions, but you don’t have to suffer in silence. Early intervention prevents complications and preserves your quality of life. If you’re experiencing leg swelling, visible varicose veins, or persistent discomfort, don’t wait for symptoms to worsen.
Schedule a consultation with experienced vascular specialists who can provide personalized treatment recommendations. Advanced diagnostic tools and proven therapies offer hope for symptom relief and improved circulation. Your legs carry you through life, give them the expert care they deserve.
Ready to take the first step toward healthier legs? Visit a board certified vascular surgeon who specializes in comprehensive venous disease management. Professional evaluation can identify problems early when treatment is most effective. Don’t let venous disease limit your activities or compromise your wellbeing. Expert help is available to restore your comfort and confidence.
Recent Posts
-
10 Daily Habits That Help Prevent Varicose Veins Naturally
February 23, 2026 -

7 Tips for Healthy Legs During Long-Distance Travel
February 9, 2026 -

How to Reduce Leg Swelling (Edema) Fast at Home: 7 Proven Methods
February 2, 2026 -
10 Anti-Inflammatory Foods That Protect Your Blood Vessels
January 21, 2026 -

5 Signs of Poor Circulation and How to Fix It
January 15, 2026 -

15 Yoga Poses to Improve Blood Circulation in Your Legs
January 9, 2026 -

10 Things You Can Do Today for a Healthier Heart and Better Flow
January 7, 2026 -

7 Effective Exercises for Chronic Venous Insufficiency
December 23, 2025 -

10 Superfoods That Improve Your Blood Circulation Naturally
December 23, 2025 -

Blood Clot in Leg Treatment in Houston: Expert DVT Care 2026
December 19, 2025 -
How Laser Ablation Can Help with Chronic Pain: Houston’s Leading Solutions
December 8, 2025 -

How Diabetes Affects Your Vascular Health
December 3, 2025 -

What Causes Varicose Veins in Your Legs?
December 3, 2025 -

Top 5 Signs You Need to Consult the Best Doctor for Vascular Surgery
December 3, 2025 -

Top 10 Vascular Surgeons in Texas: A Comprehensive Guide
December 3, 2025 -

5 Key Factors to Consider When Choosing the Best Vein Specialist
November 3, 2025 -

The Causes, Symptoms, and Treatments of Peripheral Venous Disease
November 3, 2025 -

Expert Limb Preservation Services in Houston Hospitals
November 3, 2025 -

Top 5 Vein Specialists in Houston: Expert Guide 2026
November 3, 2025 -
What Should I Expect During Pulmonary Embolism Treatment in 2026
September 30, 2025 -

Top 10 Vascular Surgeons in Texas | Best Vascular Specialists 2025
September 12, 2025 -

Choosing Minimally Invasive Vascular Surgery: A Comprehensive Guide
September 11, 2025 -

Top 5 Houston Vascular Surgeons for Effective Vein Care
August 26, 2025 -

Top 5 Signs You Need to See a Vascular Surgeon in Houston
August 19, 2025 -

How to Choose the Best Vascular Surgeon in Houston: A Complete Guide
August 18, 2025 -

Understanding Vascular Health: When to See a Specialist Like Dr. Desai
July 28, 2025 -

Why Do I Need to See a Vascular Surgeon for PAD?
July 21, 2025 -

Top 5 Signs It’s Time for Varicose Vein Treatment
July 7, 2025 -
How Smoking Affects Your Vascular Health? Discover the Risks of AAA, PAD, and Stroke
July 4, 2025 -
Preventing Strokes with TCAR: Revolutionary Treatment Now Available in Cypress
June 23, 2025 -

Minimally Invasive Vascular Surgery: Advanced Treatments for Complex Conditions
June 16, 2025 -

Peripheral Arterial Disease (PAD): What You Need to Know About Symptoms and Treatment
June 10, 2025 -

How Endovenous Laser Ablation is Changing Varicose Vein Treatment in Cypress
June 5, 2025 -

Best Vascular Surgeons in Houston: How to Choose the Right Specialist
June 5, 2025 -

Houston’s Best Varicose Vein Treatments: Expert Advice for Vascular Health
March 10, 2025 -

Meet Dr. Neil Desai: Cypress’s Trusted Vascular Surgery Expert
March 10, 2025 -
Top Solutions for Varicose Veins: Finding the Best Treatment in Houston
March 10, 2025
Contact Us
Important Links
Practice Location
- © Dr. Neil Desai, Vascular Surgeon Cypress, Houston, TX