Why Do I Need to See a Vascular Surgeon for PAD?
Peripheral Artery Disease (PAD) is a common and often serious condition that affects millions of people worldwide. It occurs when the arteries that carry blood to the limbs become narrowed or blocked, leading to reduced blood flow to the legs and feet. The condition can cause pain, fatigue, and difficulty walking, and, if left untreated, can lead to severe complications such as limb loss. That’s why seeing a vascular surgeon for PAD is crucial. Vascular surgeons are experts in diagnosing, treating, and managing vascular diseases like PAD, and they play a pivotal role in helping patients improve their quality of life and prevent the progression of the disease.
What is Peripheral Artery Disease (PAD)?
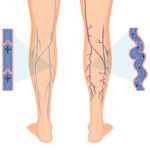
Before diving into the role of a vascular surgeon, it’s important to understand what PAD is and how it affects the body. PAD occurs when the arteries become narrowed due to the buildup of fatty deposits, also known as plaque, on the arterial walls. This condition restricts blood flow, particularly to the legs and feet, and can lead to symptoms like leg pain, cramping, and a feeling of fatigue when walking or exercising. In more severe cases, PAD can lead to critical limb ischemia (CLI), which is a serious condition characterized by severe pain, non-healing ulcers, and the potential need for amputation.
Why Should I See a Vascular Surgeon for PAD?
Vascular surgeons are medical specialists trained to diagnose and treat diseases of the arteries, veins, and lymphatic system. When it comes to PAD, vascular surgeons are uniquely qualified to evaluate, manage, and treat the disease in a way that general practitioners or cardiologists may not be equipped to do. Below are several key reasons why you should consider consulting a vascular surgeon if you have PAD or are at risk for developing it.
1. Accurate Diagnosis and Assessment
One of the most important reasons to see a vascular surgeon for PAD is their expertise in diagnosing the condition. Vascular surgeons use a combination of clinical evaluations and advanced diagnostic tools to accurately determine the presence and severity of PAD.
- Specialized Vascular Labs: Vascular surgeons use advanced vascular labs to assess blood flow and detect blockages. These labs utilize high-tech imaging and diagnostic equipment, such as ultrasound, CT angiography, and MRI scans, to visualize the arteries and determine the extent of any narrowing or blockages. In some cases, the surgeon may perform angiography, a procedure where a contrast dye is injected into the arteries to get a clear view of blood flow and any obstructions.
- Non-invasive Diagnostic Tools: The surgeon may also use non-invasive tests, such as the Ankle-Brachial Index (ABI) test, to check for PAD. This simple and quick test compares blood pressure in the ankle with the blood pressure in the arm, helping to identify blockages or narrowing in the arteries of the legs.
The ability to accurately diagnose PAD and assess its severity is critical for developing an effective treatment plan. Without a proper diagnosis, the risk of complications increases, and the disease can progress to a more severe stage.
2. Comprehensive Treatment Planning
Once PAD is diagnosed, a vascular surgeon will develop a comprehensive treatment plan tailored to your specific condition. PAD treatment is not one-size-fits-all, and vascular surgeons are skilled in creating individualized plans that address the unique needs and symptoms of each patient.
The treatment plan may include a combination of lifestyle modifications, medications, and medical procedures, all aimed at improving blood flow, reducing symptoms, and preventing further progression of the disease.
3. Medications for PAD Management
While PAD cannot be fully reversed, vascular surgeons can prescribe medications to help manage the disease and alleviate its symptoms. Medications may include:
- Cholesterol-lowering drugs: Statins or other medications may be prescribed to reduce cholesterol levels and prevent plaque buildup in the arteries.
- Blood pressure medications: High blood pressure is a major risk factor for PAD. Medications to control blood pressure may be prescribed to prevent further damage to the blood vessels.
- Diabetes management: If you have diabetes, controlling your blood sugar levels is crucial in preventing PAD progression. Vascular surgeons may work with your primary care doctor to ensure that your diabetes is well-managed.
- Antiplatelet medications: These medications, such as aspirin or clopidogrel, can help prevent blood clots, which can worsen PAD by further obstructing blood flow.
By prescribing the appropriate medications, vascular surgeons help manage PAD symptoms and reduce the risk of complications such as heart attack or stroke.
4. Lifestyle Changes
In addition to medications, vascular surgeons emphasize the importance of making lifestyle changes to manage PAD. These lifestyle modifications can significantly reduce symptoms and improve overall vascular health. Common recommendations include:
- Smoking cessation: Smoking is one of the leading risk factors for PAD, as it damages blood vessels and accelerates plaque buildup. A vascular surgeon will strongly advise quitting smoking and may offer resources or programs to help you stop.
- Regular exercise: Physical activity, particularly walking, can improve circulation and help manage PAD symptoms. A vascular surgeon will often recommend a tailored exercise program to improve your mobility and reduce pain.
- Healthy diet: A balanced diet that is low in saturated fats, high in fiber, and rich in fruits and vegetables can help control cholesterol levels and prevent further vascular damage.
- Weight management: Maintaining a healthy weight is crucial for managing PAD, as excess weight can worsen circulation and put added stress on the cardiovascular system.
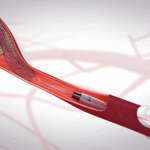
5. Minimally Invasive Procedures
For patients with more advanced PAD, vascular surgeons may recommend minimally invasive procedures to improve blood flow. These procedures are less invasive than traditional surgery and can often be performed on an outpatient basis, leading to faster recovery times.
- Angioplasty: This procedure involves using a balloon catheter to open up narrowed or blocked arteries, improving blood flow to the affected areas. In some cases, a stent (a small mesh tube) is placed in the artery to keep it open.
- Atherectomy: In this procedure, a catheter with a rotating blade or laser is used to remove plaque buildup from the arteries, further improving blood flow.
- Endovenous laser treatment (EVLT): For patients with varicose veins or chronic venous insufficiency, EVLT uses laser energy to seal off the affected veins and improve circulation.
These minimally invasive treatments can provide significant relief for patients with PAD, reducing symptoms and helping to prevent further complications.
6. Open Surgery for Severe Cases
In some cases, PAD may progress to a more advanced stage where minimally invasive procedures are no longer effective. When this occurs, vascular surgeons are skilled in performing open surgery to restore blood flow. These procedures may include:
- Bypass surgery: If an artery is severely blocked, a vascular surgeon may perform bypass surgery, where a graft is used to reroute blood flow around the blockage. This procedure is often necessary for patients with critical limb ischemia (CLI), a severe form of PAD that can lead to amputation.
- Endarterectomy: In certain situations, the surgeon may perform an endarterectomy, which involves removing plaque buildup directly from the artery to restore blood flow.
While these surgeries are more invasive, they can be life-saving and prevent the need for amputation.
7. When to See a Vascular Surgeon for PAD
It’s important to seek medical attention as soon as possible if you experience any symptoms of PAD. Early intervention can help prevent the disease from progressing to more severe stages. Some common signs that indicate the need to see a vascular surgeon for PAD include:
- Leg pain: Pain, cramping, or fatigue in the legs that occurs during walking or exercise but improves with rest (claudication).
- Rest pain: Severe pain in the legs that occurs even when you are at rest, which is a sign of more advanced PAD or critical limb ischemia.
- Non-healing wounds or ulcers: Open sores on the legs or feet that do not heal, a sign of inadequate blood flow to the area.
- Numbness or weakness: A feeling of numbness or weakness in the legs that affects your ability to walk or move.
- Cold or discolored legs or feet: If your legs or feet feel cold to the touch or are discolored (pale, blue, or red), this can indicate a lack of adequate blood flow.
Even if you do not have symptoms but have risk factors for PAD (such as smoking, diabetes, high blood pressure, or a family history of vascular disease), it’s a good idea to consult a vascular surgeon for early screening and prevention.
Conclusion
Vascular surgeons play a crucial role in the management of PAD. They offer a range of diagnostic tools, treatments, and surgical options that can significantly improve blood flow, alleviate symptoms, and prevent serious complications. If you have PAD or are at risk for developing it, seeing a Vascular Surgeon Houston is an essential step in ensuring that the disease is properly diagnosed and treated. With their specialized knowledge and expertise, vascular surgeons can help you take control of your vascular health and live a more active, pain-free life.
Recent Posts
-
10 Daily Habits That Help Prevent Varicose Veins Naturally
February 23, 2026 -

7 Tips for Healthy Legs During Long-Distance Travel
February 9, 2026 -

How to Reduce Leg Swelling (Edema) Fast at Home: 7 Proven Methods
February 2, 2026 -
10 Anti-Inflammatory Foods That Protect Your Blood Vessels
January 21, 2026 -

5 Signs of Poor Circulation and How to Fix It
January 15, 2026 -

15 Yoga Poses to Improve Blood Circulation in Your Legs
January 9, 2026 -

10 Things You Can Do Today for a Healthier Heart and Better Flow
January 7, 2026 -

7 Effective Exercises for Chronic Venous Insufficiency
December 23, 2025 -

10 Superfoods That Improve Your Blood Circulation Naturally
December 23, 2025 -

Blood Clot in Leg Treatment in Houston: Expert DVT Care 2026
December 19, 2025 -
How Laser Ablation Can Help with Chronic Pain: Houston’s Leading Solutions
December 8, 2025 -

How Diabetes Affects Your Vascular Health
December 3, 2025 -

What Causes Varicose Veins in Your Legs?
December 3, 2025 -

Top 5 Signs You Need to Consult the Best Doctor for Vascular Surgery
December 3, 2025 -

Top 10 Vascular Surgeons in Texas: A Comprehensive Guide
December 3, 2025 -

5 Key Factors to Consider When Choosing the Best Vein Specialist
November 3, 2025 -

The Causes, Symptoms, and Treatments of Peripheral Venous Disease
November 3, 2025 -

Expert Limb Preservation Services in Houston Hospitals
November 3, 2025 -

Top 5 Vein Specialists in Houston: Expert Guide 2026
November 3, 2025 -
What Should I Expect During Pulmonary Embolism Treatment in 2026
September 30, 2025 -

Top 10 Vascular Surgeons in Texas | Best Vascular Specialists 2025
September 12, 2025 -

Choosing Minimally Invasive Vascular Surgery: A Comprehensive Guide
September 11, 2025 -

Top 5 Houston Vascular Surgeons for Effective Vein Care
August 26, 2025 -

Top 5 Signs You Need to See a Vascular Surgeon in Houston
August 19, 2025 -

How to Choose the Best Vascular Surgeon in Houston: A Complete Guide
August 18, 2025 -

Understanding Vascular Health: When to See a Specialist Like Dr. Desai
July 28, 2025 -

Why Do I Need to See a Vascular Surgeon for PAD?
July 21, 2025 -

Top 5 Signs It’s Time for Varicose Vein Treatment
July 7, 2025 -
How Smoking Affects Your Vascular Health? Discover the Risks of AAA, PAD, and Stroke
July 4, 2025 -
Preventing Strokes with TCAR: Revolutionary Treatment Now Available in Cypress
June 23, 2025 -

Minimally Invasive Vascular Surgery: Advanced Treatments for Complex Conditions
June 16, 2025 -

Peripheral Arterial Disease (PAD): What You Need to Know About Symptoms and Treatment
June 10, 2025 -

How Endovenous Laser Ablation is Changing Varicose Vein Treatment in Cypress
June 5, 2025 -

Best Vascular Surgeons in Houston: How to Choose the Right Specialist
June 5, 2025 -

Houston’s Best Varicose Vein Treatments: Expert Advice for Vascular Health
March 10, 2025 -

Meet Dr. Neil Desai: Cypress’s Trusted Vascular Surgery Expert
March 10, 2025 -
Top Solutions for Varicose Veins: Finding the Best Treatment in Houston
March 10, 2025
Contact Us
Important Links
Practice Location
- © Dr. Neil Desai, Vascular Surgeon Cypress, Houston, TX